Abstract
Background:
Inflammatory bowel disease (IBD) patients are three times more likely to develop venous thromboembolism (VTE) compared to the general population, especially during disease flares and while hospitalized. Current guidelines recommend prophylaxis during all hospitalizations, though data are sparse. In this systematic review and meta-analysis, we sought to pool all existing data on the efficacy and safety of VTE prophylaxis in hospitalized IBD patients.
Methods:
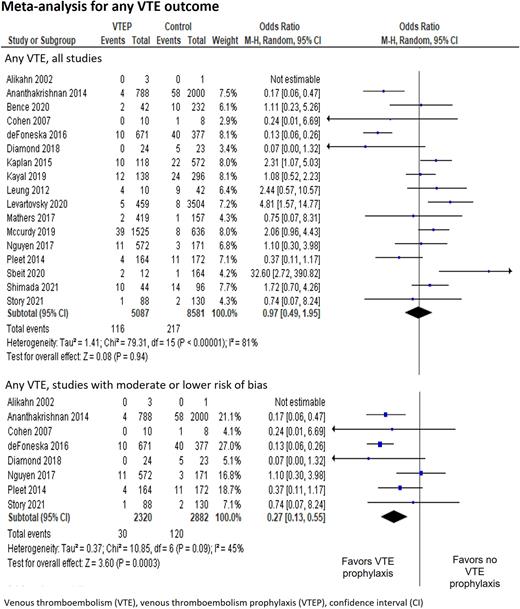
We performed a systematic review and meta-analysis. We searched MEDLINE and other databases up to 2/2022, for studies reporting on hospitalized IBD patients (both adult and pediatric, in medical or surgical wards), who were treated with non-therapeutic dose anti-coagulation during hospitalization, compared to no prophylaxis. Our primary efficacy outcome was any VTE (deep vein thrombosis, portomesenteric vein thrombosis, catheter-related thrombosis, and pulmonary emboli), and the primary safety outcome used was major bleeding. Results were pooled using a random-effects model meta-analysis. Odds ratios (OR) and 95% confidence intervals (CI) were calculated. Risk of bias was assessed with the ROBINS-I tool and the Cochrane Collaboration's tool for randomization method.
Results:
We were able to extract data from 18 observational studies, and 2 subgroups from randomized trials, published between 2003 and 2021. The studies were highly variable regarding the study populations, interventions, and outcome definitions, as well as methodological quality. Meta-analysis of all studies did not show a significant effect of prophylaxis on VTE events (OR 0.97 [95% CI 0.49-1.95]). A sensitivity analysis of 8 studies with moderate or lower risk of bias showed a statistically significant reduction in VTE events (OR 0.27 [95% CI 0.13-0.55), with a number needed to treat (NNT) of 35 (95% CI 26.8-49.8). Among studies with lower risk of bias, a significant protective effect of VTE prophylaxis persisted in subgroup analyses of long-term follow up VTEs (OR 0.24 [95% CI 0.08-0.69]), of adult patients only (OR 0.27 [95% CI 0.12-0.61]), and of a mixed population of surgical and medical patients (OR 0.37 [95% CI 0.19-0.74]). Major bleeding was reported in three studies classified with moderate or lower risk of bias, and meta-analysis showed a significantly increased risk in the prophylaxis group (OR 2.02 [95% CI 1.11-3.67], number needed to harm (NNH) of 114 (95% CI 40.7-very large number).
Discussion:
The main analysis did not show a reduction in VTE events in hospitalized IBD patients treated with prophylaxis. However, in studies with lower risk of bias, a protective benefit of prophylaxis consistent across several subgroups was shown (NNT=35), which should be carefully considered against an increased risk of major bleeding (NNH=114). Currently available data is limited, and mostly retrospective, and randomized controlled trials dedicated to hospitalized IBD patients are needed before universal VTE prophylaxis can be recommended.
Disclosures
Gafter-Gvili:Pfizer: Honoraria, Other: honoraria for lectures and advisory board ; Bayer: Honoraria, Other: honoraria for lectures and advisory board ; Sanofi: Honoraria, Other: honoraria for lectures and advisory board ; Medison: Honoraria, Other: honoraria for lectures and advisory board .
Author notes
Asterisk with author names denotes non-ASH members.